WellSpark Health, a leading disease prevention and management company, is helping employers improve the health of their organization and people. WellSpark recently authored a white paper that looks at actionable steps companies can take to address the racial disparities in healthcare services that employees may face.
Nearly 20 years ago the National Academy of Medicine, formerly known as the Institute of Medicine, published “Unequal Treatment” documenting racial and ethnic disparities in healthcare and recommendations for fixing them. The COVID-19 pandemic pushed the issue of equity in healthcare to the forefront with stark daily counts of infections, hospitalizations, and deaths among people of color. Everyone seems to agree: it’s time for action. Employers, here’s how you play a role.
A New Angle on Diversity, Equity, and Inclusion: Addressing racial disparities that impact employee health
By Wayne Rawlins, M.D., M.B.A. and Andi Campbell, M.S.
Many recognize their stake in improving the U.S. healthcare system and are active in exercising it among policymakers, healthcare providers, and insurers. Employers provide health insurance for nearly 50% of the U.S. population.
For some employers though, the COVID-19 pandemic revealed unsettling facts about inequities in care, treatment, and mortality experienced by their employees of color. Calls for racial justice now include demands to move further and more quickly toward equity in healthcare.
This may leave you, as an employer, wondering:
- What is our role beyond providing health insurance and wellness programs?
- Do we have a responsibility to employees who don’t qualify for coverage?
- Will my employees be willing to help us examine this — or will it cause friction and undermine our success as we emerge from lockdown?
- How does this impact the work we are already doing for diversity, equity, and inclusion?
JP Morgan Chase shot a signal to the sky when it announced recently that it is founding a new business unit, Morgan Health, bent on improving “the quality, efficiency, and equity of employer-sponsored health care.” Its first customers: JP Morgan Chase’s own employees and dependents.
Many employers don’t have JP Morgan Chase-size resources. But there are ways that employers with fewer resources (but equal resolve) can address racial disparities in healthcare. Let’s examine where COVID-19 has brought us in healthcare and some ways you can be a force for influencing change.
What we learned about racial disparities from the COVID-19 pandemic
COVID-19 created a public health crisis — and an especially virulent crisis for communities of color. Black, Latinx, Pacific Islander, and Indigenous people have contracted the virus, been hospitalized, and died from it at higher rates than Whites. Look at one startling statistic for mortality.
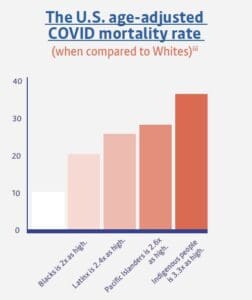
Black is 2x as high | Latinx is 2.4x as high | Pacific Islanders is 2.6x as high | Indigenous people is 3.3x as high
The National Academy of Medicine report of 2003, and subsequent studies, have found that racial inequities in healthcare persist even when adjusting for variables such as income and education. A recent article in Kaiser Health News, “Racism Derails Black Men’s Health, Even as Education Levels Rise,” quoted a prominent researcher:
“No matter how far you go in school, no matter what you accomplish, you’re still a Black man,” said Derek Novacek, who has a doctorate in clinical psychology from Emory University and is researching Black-White health disparities at UCLA.”
The situation is equally acute in mental health. The nonprofit organization, Mental Health America, on its website, summarizes findings of multiple studies of racism in mental health services. In general, rates of mental illness among people of color are comparable to rates in Whites. Then, paths diverge when it comes to treatment and diagnosis, with people of color:
- Having less access to treatment by professionals who understand their culture and language
- A higher risk of being misdiagnosed because of the lack of cultural competency among providers
- At times avoiding treatment at all because of cultural or community norms that say it is not ok
The future of American workforce demographics
If you are an employer who offers health benefits, you may assume that those benefits improve the health of your employees, regardless of race. Unfortunately, progress isn’t as wide or as fast as we might assume, even after the implementation of the Affordable Care Act of 2010.
The National Healthcare Quality and Disparities Report, released in 2018, said that while insurance coverage has improved substantially, major disparities persist in quality and safety of care for racial and ethnic minorities and the poor and uninsured. The American Rescue Plan Act, signed by President Biden in March, attempted to reduce the ranks of uninsured with enhanced subsidies and expanded eligibility for subsidies to help pay premiums through the government marketplace in the 2021 and 2022 tax years.
The act addresses the crisis we are in right now. It contains financial relief for people without jobs or those raising children as well as pull-out-the-stops activities to get COVID-19 vaccines in arms. Racism in healthcare, however, has deep and resistant roots in structural and systemic biases and barriers. One bill cannot shatter those.
By 2060, Blacks, Hispanics, Asians, and other minorities will make up a majority of the U.S. population. Tomorrow’s workforce will be even more diverse than today’s — in gender, ethnicity, culture, race, religion, and sexual preference and identification. If disparities are not abated, then, we can assume:
- Healthcare costs will continue to rise and sap resources that could otherwise be returned in investment or profit
- Workforce productivity will languish and lag behind that of other countries.
- Health outcomes will worsen for a growing proportion of the working population
What employers can do
Wondering where to start in addressing racial disparities in healthcare?
Here’s the approach that we suggest with some thoughts on how to manage it.
Start with gaining a deeper understanding of your workforce’s sociodemographic characteristics.
Do you have a significant employee population of a specific ethnic or racial identity? If this data isn’t readily available, consider the geographical implications of your employee population.
Some regions, because of their industries or past immigration patterns, have large populations with similar backgrounds. You could use information that is available publicly, such as average salary or cost-of-living for regions, cities, or zip codes to make meaningful assumptions.
Understand your workforce demographics > Explore data about their health and wellbeing > Write your action plan > Measure results. Tweak and try again
One word of caution: making assumptions based on address or surname can be inaccurate. Dr. Rawlins, for example, has a name and address that indicate with 96% probability that he is White (he is not).
Therefore, it is important not to implement outreach to a specific individual based solely on statistically imputed information.
Then, dive deeper.
In addition to socioeconomic characteristics, select other key data points for your employees and their dependents. Some of those relevant data points may be:
Access to care: Do they have health insurance? Do they have a usual primary care provider?
Utilization patterns: Do they have health exams? Do they get vaccinations (including the COVID-19 vaccine)? Do they take their prescription medicines?
Quality measures: Do they have a healthcare provider who treats them with respect? Have they used the emergency room for routine care? Have they been admitted to the hospital for chronic disease? (asthma, for example?)
Personal finances: Have they potentially forgone care, medications, or treatment because of cost?
Make sure you have these conversations with employees across your entire organization, regardless of whether or not they are enrolled in your health plan. Partner with your health broker or use a risk stratification tool to identify—whenever possible—the disparities in care and treatment for members of racial or ethnic minorities. Make sure you have these conversations with employees across your entire organization, regardless of whether
The Health Research and Educational Trust (HRET) Disparities Toolkit is a good, web-based resource for systematically collecting race, ethnicity, and primary language data. There is information in the toolkit about how to engage communities—in your case, employees and dependents—in conversations that can enrich your study and your improvement efforts. Leading focus groups about how your company can more effectively support its minority employees is a way to encourage employees to volunteer information about their healthcare experiences that may be useful.
With data in hand, work up your action plan
Don’t assume this is your job alone. In fact, you probably can find allies among these groups:
- Employees themselves: You may already have employee working groups that address other workplace issues, including diversity, equity, and inclusion. Tack health inequity onto conversations that are already underway. Take advantage of employee resource groups with similar cultural identities to the communities you are trying to engage.
- Community activists and leaders: With concentrated communities of color, there may be businesses, institutions (such as places of worship or schools), or leaders outside of the healthcare system who can work with It’s important to remember that to people who live with discrimination, information sources matter.
- Other businesses: The greater Seattle area, where Rawlins lives, was the first region hit hard by COVID-19. Executives from major corporations and healthcare leaders worked together with government officials to address the crisis. While many of those people may have otherwise competed for customers or had major differences on policy in the past, they united in the crisis.
- Innovators and thought leaders: You likely belong to industry, business, or trade Other groups may have already started to tackle the issue of racial disparities in healthcare—or would leap at the chance to work together. The Business Group on Health has Innovator Awards in Advancing Health Equity. Remember, there is no monopoly on ideas when people’s health is at stake.
Be transparent with your employees: Let them know your intentions. Use your regular communication channels — town halls, newsletters, intranets, department meetings, leadership calls — to share what you are doing and why.
Measure the effectiveness of your actions
When you set out, it’s important to envision what success looks like for your organization so you can design your plan. Will you measure success by:
- Better understanding among employees of the importance of health and wellbeing?
- Higher engagement in programs designed to improve wellness and health outcomes?
- Verifiable behavior change in self-care and wellbeing?
Keep in mind that even the smallest progress could save an employee’s life. As you move through the work, tweak your programs. Continue to brainstorm ideas and test them. This is not a one or even a five-year plan (although you can certainly get results in that much time). Systemic racism has a history of more than 400 years in the United States.
Final thoughts
Lastly, it’s important when socializing plans with senior leaders to be upfront that your effort to address racial disparities can potentially mean higher medical costs in the short term. If people begin to seek primary care, take maintenance medicines, and get their lab tests, they may incur claims that you could have to pay.
That said, evidence supports that when companies cultivate a culture of wellbeing and employees engage in preventive care, the cost of claims improves long-term. So, an investment today could dramatically save money tomorrow.
All of this reminds us of the fable of the youngster tossing starfish stranded on a beach back into the sea before the tide receded and they were left to die.
A passerby points out that the youngster cannot possibly save all the starfish—there are too many, the beach is too large.
The youngster picks up another, tosses it into the surf, and says, “I made a difference for that one.”
We are optimistic. Coming out of a tumultuous 2020, people are ready for something different. Employers have a unique opportunity to blend wellbeing and diversity efforts into a force that can inspire change and, more importantly, save lives.
May we help?
WellSpark Health moves disparate, long-tenured employee populations along a path toward a more enduring well. With our life-dimensional approach, employees come to understand that WellSpark will help them discover for themselves what actions they are willing and able to take. And by steadily building upon one change—one success—after another, WellSpark creates enduring results that positively impact both employees and their employers.
To reach us and talk over how we can help you address racial inequities in your employees’ healthcare, visit wellsparkhealth.com or email info@wellsparkhealth.com.
ABOUT THE AUTHORS
Andi Campbell, M.S.
As the Chief Growth Officer for WellSpark Health, Andi is responsible for developing and delivering holistic,
“total person” wellbeing programs to thousands of employees across the country. She is a progressive leader and an experienced senior human resources executive who was previously Senior Vice President, Head of People + Culture for LAZ Parking, one of the largest parking companies in the world. Find accolades for Andi’s work with people strategies in CLO, ELearning, Parking and TD Magazine.
She was named one of the Top Young Trainers by Training Magazine in 2012 and was recognized with a “Game Changer” award by Workforce Magazine in 2014. You can hear Andi’s passion for people in her TEDx Hartford talk from 2017 or her DisruptHR talk from 2018.
Recognized as the Women in Parking Impact Award winner in 2020, Andi is also a registered yoga teacher, certified Intuitive Coach, Integrative Nutrition Health Coach and black belt in Tang Soo Do. She has a master’s degree in Industrial/Organizational Psychology and a bachelors degree in English.
Wayne Rawlins, M.D., M.B.A.
Dr. Rawlins is Chief Medical Officer at WellSpark Health. In this role he is responsible for health, prevention and wellbeing strategy and value demonstration at WellSpark. Previously, he was the Vice President and Chief Medical Officer at ConnectiCare, a leading health plan serving the residents of Connecticut. He has also held senior clinical leadership positions at a large national health insurer.
A leading immunization expert, Dr. Rawlins served as a member of the National Vaccine Advisory Committee, where he worked with the U.S. Department of Health and Human Services to advise and make recommendations on national vaccine policy. Dr. Rawlins is noted as a vaccine financing subject matter expert.
A specialist in health equity and resolving health disparities, Dr. Rawlins serves on the COVID, medical advisory, and health equity committees of the National Alliance of Healthcare Purchasers Coalition. He is also a member of the NCQA Committee on Performance Measurement.
He received his medical degree from the University of Connecticut, completed an internal medicine residency and chief residency at the University of Rochester in New York, and received a master’s in business administration from Rensselaer Polytechnic Institute. Dr. Rawlins is board certified in internal medicine. He was a physician manager and practicing physician treating patients in a primary care practice for more than a decade.
